Starting an IVF journey can feel like a rollercoaster—exciting but a little scary. But guess what? Learning about embryo and how they grow can turn that fear into confidence! Let’s break down everything you need to know, step by step, using simple words and fun examples.
What’s an Oocyte? (The “Egg Cell”)
The Basics of an Oocyte
An oocyte is just a fancy name for an egg cell. Think of it like a tiny “seed” in a woman’s ovaries. This seed is one of the largest cells in the human body—about the size of a grain of sand! For a baby to form, this seed needs to meet a sperm cell.
Fun Fact: Women are born with all the oocytes they’ll ever have—about 1-2 million! By puberty, only 300,000 remain, and only 400-500 will mature in a lifetime.
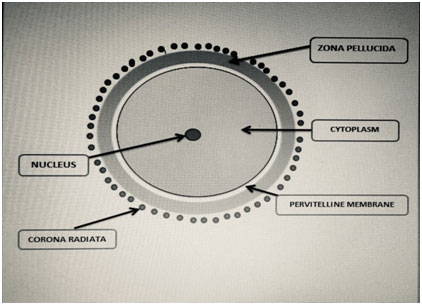
Parts of an Oocyte (Like a Mini Spaceship!)
Doctors check oocytes carefully during IVF. Here’s what they look at:
- Corona Radiata:
- A fluffy, nutrient-rich layer around the egg.
- Acts like a “food delivery service” for the egg.
- Zona Pellucida:
- A thick, protective outer shell (like a spaceship’s armor!).
- After fertilization, this shell hardens to block other sperm.
- Vitelline Membrane:
- The egg’s “skin” that holds everything together.
- Nucleus:
- The “brain” of the cell—holds all the genetic instructions (DNA).
- Cytoplasm:
- Jelly-like fluid that keeps the cell healthy.
Why Oocyte Quality Matters
Not all oocytes are the same. Doctors grade them based on:
- Shape: Round is best!
- Layers: Fluffy corona radiata = healthy.
- No Damage: Cracks or dark spots mean lower quality.
Grade A Oocyte: Perfect shape, fluffy layers, no damage.
Grade B Oocyte: Slightly uneven shape or thinner layers.
The Journey from Oocyte to Embryo
Fertilization: When Sperm Meets Egg
During IVF, doctors mix sperm and oocytes in a lab dish. If a sperm breaks through the zona pellucida, fertilization happens!
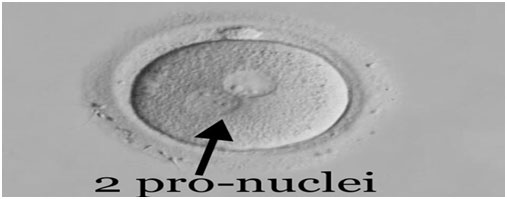
- 2PN (Two Pro-Nuclei):
- 18–19 hours after fertilization, the egg and sperm nuclei fuse.
- This forms a zygote (fertilized egg).
Embryo Development: Day-by-Day Breakdown
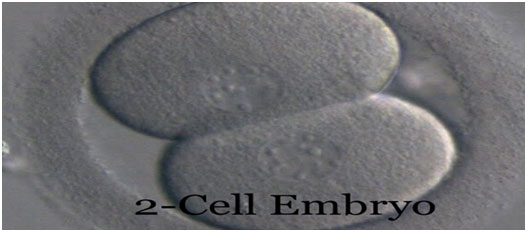
Day 1: 2-Cell
- 24–30 hours after fertilization, the zygote splits into 2 cells.
- Doctors check if cells are equal in size.
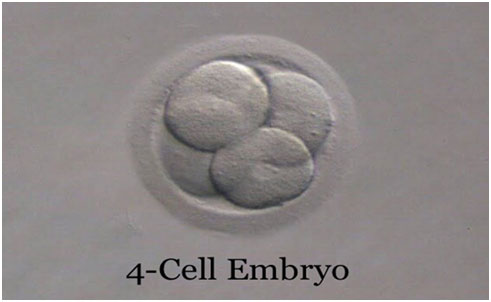
Day 2: 4-Cell
- By 40 hours, it splits into 4 cells.
- Uneven cells or fragments (tiny broken pieces) mean lower quality.
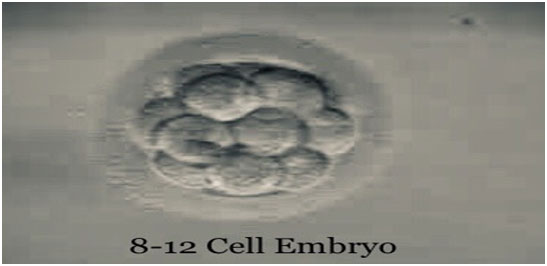
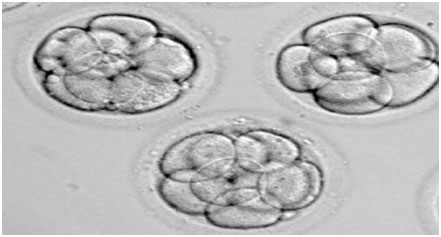
Day 3: 8-Cell
- Around 68 hours, it has 6–12 cells.
- This stage is critical—if cells divide too slowly, the embryo might not survive.
Day 4: Morula Stage (Like a Raspberry!)
- A solid ball of 16+ cells form.
- Named “morula” (Latin for “mulberry”) because it looks like a tiny berry!

Day 5: Blastocyst Stage (The Big Upgrade!)
- A fluid-filled cavity forms, turning the morula into a blastocyst.
- Has two parts:
- Inner Cell Mass (ICM): Becomes the baby.
- Trophectoderm (TE): Forms the placenta.
Why Day 5 Matters: Blastocysts have a higher chance of implanting in the uterus.

Grading Embryos—Like Report Cards!
Embryo Grading System
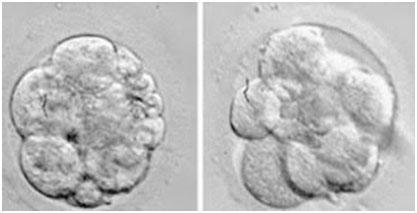
Doctors grade embryos from 1 (best) to 4 (worst):
- Grade 1:
- Cells are equal size.
- No fragments (breaks).
- Chance of Success: Highest!
- Grade 2:
- Slightly uneven cells.
- Up to 10% fragments.
- Chance of Success: Good.

- Grade 3:
- Uneven cells.
- 10–25% fragments.
- Chance of Success: Moderate.
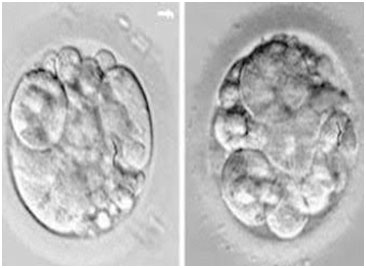
- Grade 4:
- Very uneven cells.
- 50%+ fragments.
- Chance of Success: Low.
Note: Even low-grade embryos can sometimes result in pregnancies, but higher grades are safer.
Blastocyst Grading: The A, B, C System
Blastocysts get two grades (e.g., 4AA):
- First Grade: Blastocyst size (1–4):
- 1: Early blastocyst (small cavity).
- 4: Expanded blastocyst (large and ready to hatch).
- Second Grade: Inner Cell Mass (A–C):
- A: Many tightly packed cells.
- C: Few loose cells.
- Third Grade: Trophectoderm (A–C):
- A: Many healthy cells.
- C: Few weak cells.
Example: A “4AA” blastocyst is the gold standard—large, strong ICM, and healthy TE.
Why Embryo Knowledge = IVF Power!
How Grading Affects Your IVF Success
- Higher Grades = Better implantation chances.
- Lower Grades = May need multiple IVF cycles.
Did You Know?
- Only 30–50% of embryos reach the blastocyst stage.
- Even top-grade embryos have a 60–70% chance of implanting.
Questions to Ask Your Doctor
- “What grade are my embryos?”
- “How many are reached blastocyst stage?”
- “Do you recommend transferring one or two?”
Common Myths About Embryos (Busted!)
Myth 1: “Bigger embryos are better.”
Truth: Size doesn’t matter—quality does! A small, Grade 1 embryo beats a large, Grade 3 one.
Myth 2: “All embryos can become babies.”
Truth: Only 20–30% of embryos are healthy enough to implant.
Myth 3: “IVF always works on the first try.”
Truth: Success rates vary. Younger women (under 35) have a 40–50% chance per cycle.
Tips to Improve Embryo Health
For Women
- Eat Healthy: Fruits, veggies, and proteins.
- Avoid Smoking/Alcohol: They damage oocytes.
- Manage Stress: Yoga or meditation helps.
For Men
- Healthy Sperm Matters Too! Avoid tight underwear and hot tubs.
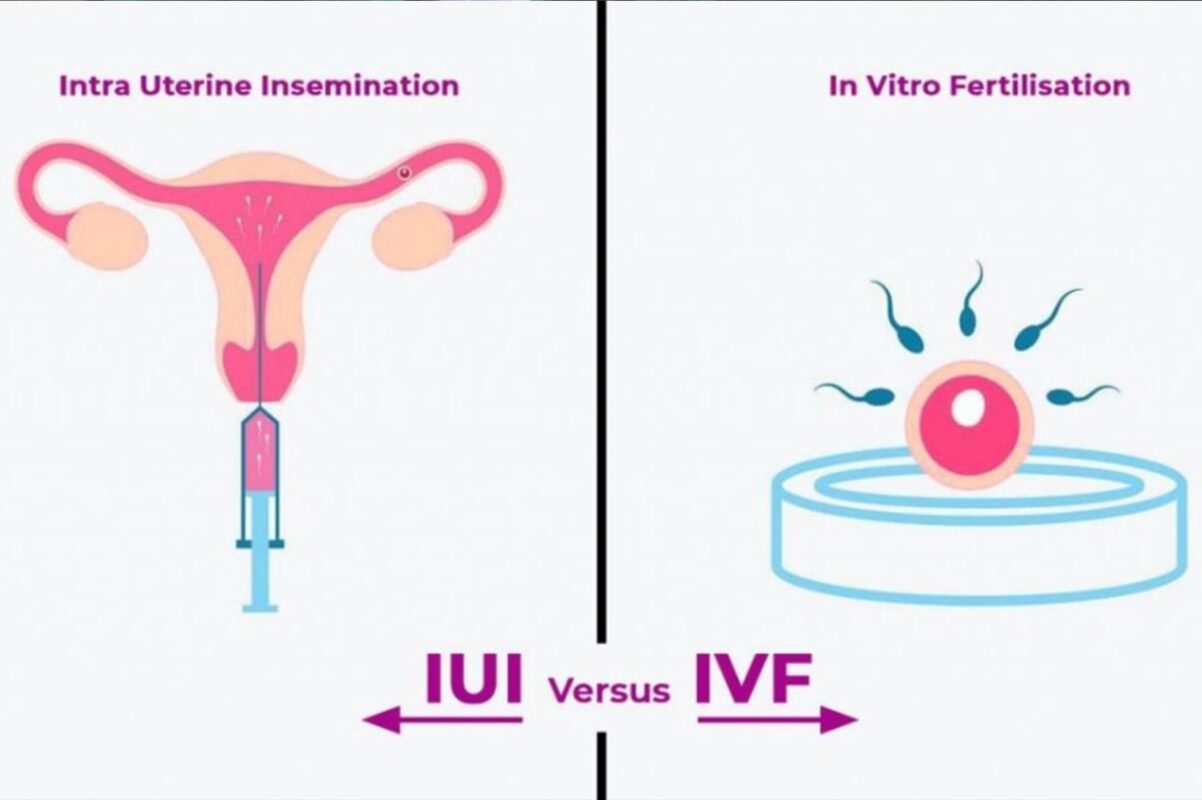
The IVF Process—Step by Step
Step 1: Ovarian Stimulation
- Hormone injections help ovaries produce multiple oocytes.
Step 2: Egg Retrieval
- Doctors collect oocytes using a tiny needle (under anesthesia).
Step 3: Fertilization
- Sperm and oocytes are mixed in a lab.
Step 4: Transfer
- The best embryo is placed into the uterus using a thin catheter.
Why Choose Pahlajanis’ IVF?
- Transparency: We explain your embryo grades clearly.
- Expertise: Our lab uses advanced technology for grading.
- Support: Chat with our team anytime—no question is too small!
FAQs (Simple Answers!)
Q: Can I see my embryo?
A: Yes! Many clinics provide photos or videos.
Q: What if all my embryos are low-grade?
A: Your doctor might suggest genetic testing or lifestyle changes.
Q: How many are transferred?
A: Usually 1–2 to avoid risky multiple pregnancies.









The manipulation and freezing of embryos in fertility treatments prompts discussions about consent, ownership, and the rights of unused embryos.Vardhan Fertility Hospital is the best test tube baby, IVF, IUI, womens care center in bangalore, India has world-class facilities, advanced procedures and equipment with high quality infertility treatment.
Thanks for breaking down embryo development so clearly! I appreciate how you explained the embryo stages, grading, and what each term means — makes IVF less scary and more understandable. Great post! hanks for sharing! Truly inspiring!
Thanks for breaking down embryo development so clearly! I appreciate how you explained the embryo stages, grading, and what each term means — makes IVF less scary and more understandable. Great post! hanks for sharing! Truly inspiring!